Understanding the Connection: Microbiome, Brain, and Mental Health
Written on
The relationship between the microbiome and mental health is a fascinating and evolving area of research.
To be clear, I am quite cautious about germs, particularly during flu season.
I often find myself sanitizing my hands or using a pencil to press elevator buttons. Yes, I’m that person. The mere mention of "bacteria" sends shivers down my spine.
My germophobia stems from a desire to avoid illness, as being unwell disrupts my productivity. However, recent research indicates that bacteria and other microbes can actually bolster our immunity against sickness.
Remarkably, there are approximately 39 trillion microbes residing in and on our bodies at this very moment. That's 9 trillion more than our own cells! (You can imagine my surprise upon learning this…)
Researchers are uncovering the crucial roles these microbes play in our health, revealing connections to various diseases, including neuropsychiatric conditions. The human microbiome could revolutionize our understanding of mental health issues and open up new avenues for treatment.
The Human Microbiome
The human microbiome encompasses all the microbes inhabiting our bodies, including bacteria, viruses, archaea, fungi, and their genetic material.
These microorganisms inhabit various parts of our body, including our skin and nasal passages, and are essential for numerous bodily functions. Some of their responsibilities include:
- Nutrient provision for our cells
- Digestive assistance
- Immune system programming
Almost every bodily function is influenced by the microbiome in some manner.
The composition of the microbiome varies from individual to individual and is influenced by factors such as diet, environment, and genetics. As we delve deeper into this captivating scientific field, we're beginning to grasp how our early life experiences shape our microbiome.
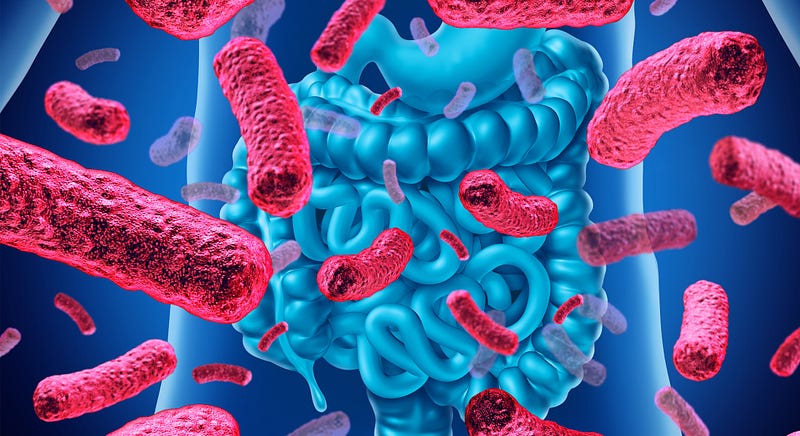
Research has shown a strong correlation between the composition of the gut microbiome and conditions like irritable bowel syndrome and diabetes.
Even more intriguing is the growing understanding of the microbiome's influence on brain health and neuropsychiatric disorders.
The Microbiome-Gut-Brain Axis
When considering mental health, the connection to the gut microbiome might not be the first thought that arises. However, research is revealing intricate communication pathways between the gut microbiome and the brain, prompting significant funding to explore this area further.
The gut and brain are linked through a biochemical communication system known as the gut-brain axis, facilitated by immune pathways and nerve cells. This connection allows the brain to send signals that can either enhance or inhibit digestion.
There are four primary modes of communication between the brain and the gut microbiome:
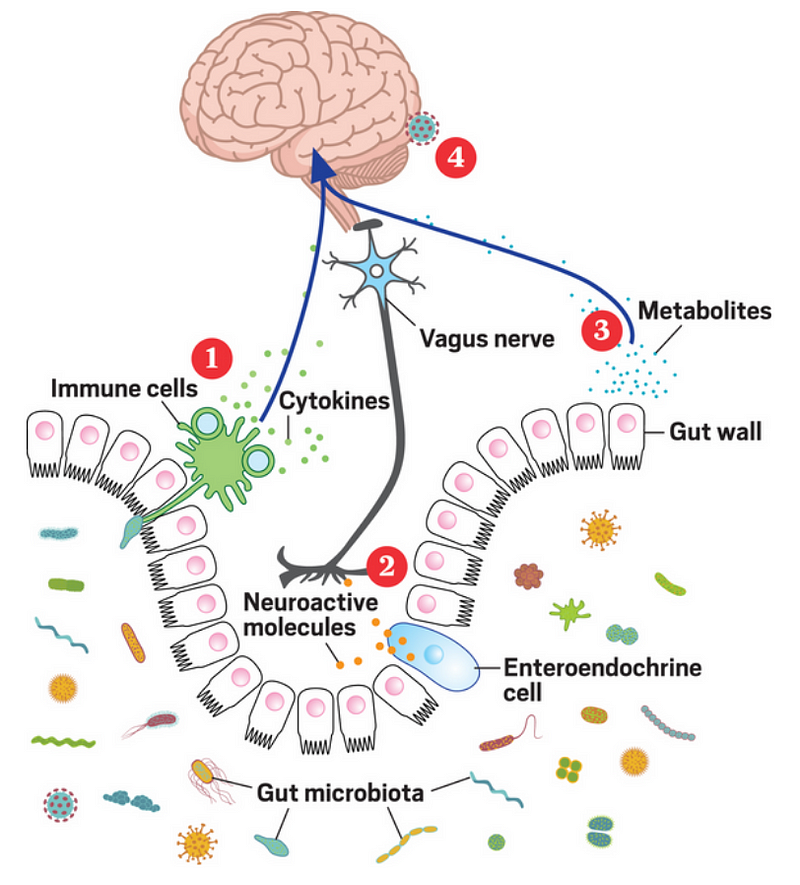
- Microbes trigger immune cells to release cytokines, which then travel to the brain.
- Microbes interact with enteroendocrine cells in the gut, producing neuroactive compounds that communicate with the brain via the vagus nerve. Notably, 80 to 90 percent of the vagus nerve's neurons relay sensory information from the gut.
- Microbes generate metabolites and neurotransmitters that can enter the brain through the blood-brain barrier.
- Interestingly, human gut bacteria have been found in brain tissue.
Our comprehension of the microbiome-gut-brain axis is continuously evolving:
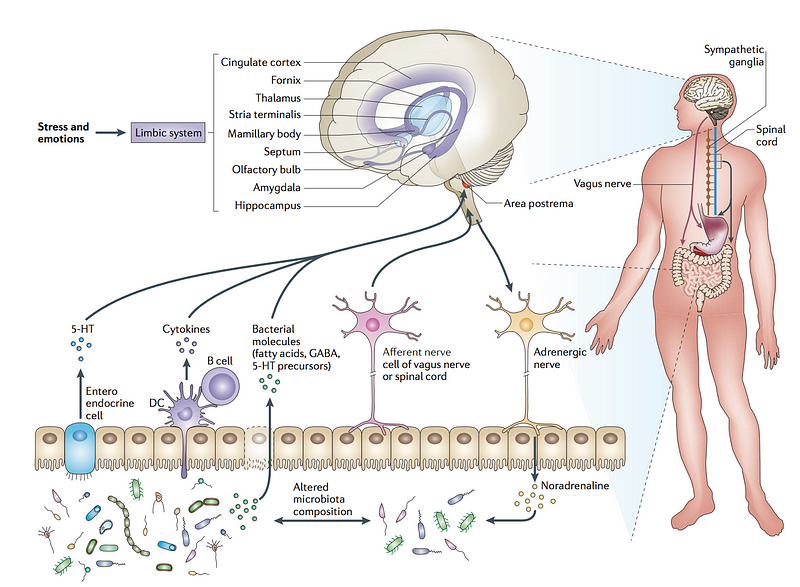
Mechanisms through which bacteria can affect brain function and behavior include:
- Bacterial products entering the brain via the bloodstream
- Cytokine release from mucosal immune cells
- Gut hormones like serotonin, released from enteroendocrine cells
- Afferent neural pathways, including the vagus nerve
The microbiome-gut-brain axis is bidirectional, indicating that the brain can also influence microbiome composition. Stress and emotional states can alter gut microbiota through the release of stress hormones, which may affect bacterial behavior and composition.
Although still in the early phases, this research is already reshaping our understanding of various neuropsychiatric disorders.
Anxiety, Depression, and Schizophrenia
Approximately 1 in 5 adults in the U.S. experience mental illness annually. However, our current scientific insights into mental health issues are limited, complicating diagnosis and treatment.
While numerous studies investigate the neurological underpinnings of mental health conditions, many fail to consider the broader physiological factors at play. Emerging research into the gut microbiome's influence on mental health is enhancing our understanding of disorders such as anxiety, depression, and schizophrenia.
Many are aware that serotonin (5-HT) regulates mood and social behavior, playing a crucial role in anxiety and depression. However, it’s essential to note that 90% of serotonin is synthesized in the gut!
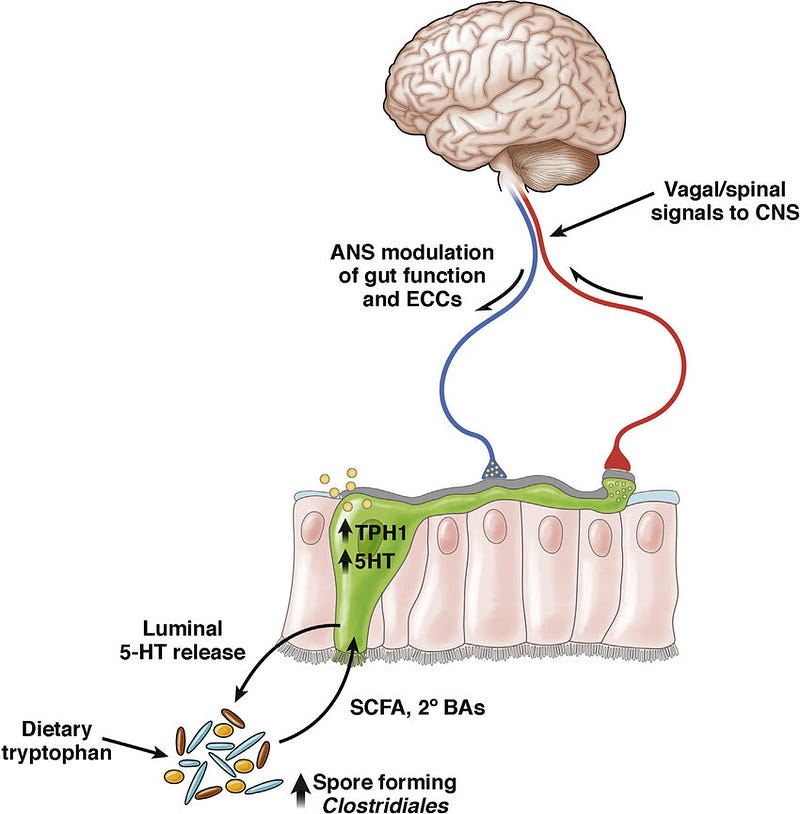
The enterochromaffin cells (ECCs) responsible for serotonin synthesis are influenced by short-chain fatty acids (SCFAs) and secondary bile acids (2BAs) from Clostridiales, which enhance ECC activity when dietary tryptophan is abundant.
These ECCs communicate with afferent neurons, such as the vagus nerve, transmitting serotonin to the brain. Additionally, the autonomic nervous system can activate ECCs, releasing serotonin into the gut, where it may interact with microbes.
Thus, it is plausible that *Clostridiales* and other gut microbes could impact anxiety and depression through this pathway.
Research has shown that mice separated from their mothers, inducing anxiety, exhibit long-term microbiome alterations.
This suggests that the gut microbiome may influence the HPA-axis, a key stress response system. Studies revealed that Lactobacillus rhamnosus JB-1, known for its immune-modulating properties, reduced stress and altered brain chemistry, resulting in decreased anxiety. Notably, this effect was absent in mice with severed vagus nerves.

Feeding Lactobacillus rhamnosus JB-1 to mice also influenced protein receptor levels in various brain regions, affecting receptors linked to depression, anxiety, and schizophrenia.
Alterations in the microbiome have been documented in patients experiencing First Episode Psychosis (FEP). The oropharyngeal microbiome of those with schizophrenia exhibited increased lactic acid bacteria, while the gut microbiome showed a rise in the phylum Proteobacteria, predominantly due to Succinivibrio. Higher levels of Lactobacillus were observed in FEP patients, correlating with symptom severity.
Further studies indicated increased prevalence of Clostridiales, Lactobacillales, and Bacteroidales, along with genera like Lactobacillus and Prevotella in FEP patients compared to healthy controls. Imaging revealed elevated choline levels in FEP patients, indicating potential cell membrane dysfunction linked to microbiome changes that may activate microglia through SCFA production.
Additional noteworthy findings include:
- Mice receiving a microbiome transplant from a depressed human exhibit depressive-like behaviors.
- A population-level study revealed that genera *Coprococcus* and *Dialister* were diminished in depression, while butyrate-producing *Faecalibacterium* and *Coprococcus* were associated with improved quality of life. Butyrate is recognized for its antidepressant properties.
- Lactobacillus helveticus R0052 has been shown to impact neurons in the hippocampus and amygdala, with increased levels reducing psychological distress.
Treatments and Opportunities
As our understanding of the microbiome-gut-brain axis advances, so too will our therapeutic approaches to mental health.
- Researchers are investigating probiotics, prebiotics, and synbiotics as potential treatments for anxiety, depression, and stress, termed "psychobiotics." Preliminary results have shown promise.
- Fecal microbiota transplants (FMT) from donors with healthy microbiomes are being explored as treatments for Alzheimer’s disease and have demonstrated mood-altering effects in mice.
- Phage therapy, utilizing bacteriophages to combat harmful bacterial infections, has shown potential in modifying the gut microbiome.
While this field is still developing, our expanding knowledge of the gut microbiome is poised to reshape our understanding of neuropsychiatric disorders and herald new diagnostic and treatment options.
Hello! I’m Mikey, an enthusiastic student intrigued by the intersections of emerging technologies, neuroscience, and mental health. My aspiration is to revolutionize the diagnosis and treatment of neurological and psychiatric conditions. I'm also interested in a wide array of topics. Feel free to reach out at [email protected] if you’d like to discuss this article, share opportunities, or chat!
Further Reading:
The Brain-Gut-Microbiome Axis
Preclinical and clinical studies have demonstrated bidirectional interactions within the brain-gut-microbiome axis. For more information, visit: www.ncbi.nlm.nih.gov